01 April, 2024
Malaria remains a significant global health concern. The transmission of malaria occurs across five WHO regions, encompassing 84 countries. The WHO European region has been malaria free since 2015. With significant progress so far, the overarching goal is to become a malaria free world 1.
Malaria Overview
Malaria is a life-threatening disease caused by parasites, transmitted to humans through the bites of infected female Anopheles mosquitoes. Malaria cannot be transmitted from person to person, but it can be transmitted via blood transfusion and through the use of contaminated needles. Malaria is preventable and curable, but it remains a major public health challenge, especially in resource-limited settings 2.
There are five species of Plasmodium parasites that causes malaria in humans: P. falciparum, P. knowlesi, P. malariae, P. ovale, and P. vivax. P. falciparum and P. vivax are the most widespread and pose the greatest threat, with P. falciparum being the deadliest of all species 2.
Symptoms of malaria range from mild to severe and may include: breathing difficulties, chills, confusion, fatigue, fever, headache, and seizures. Severe cases, particularly those caused by Plasmodium falciparum (P. falciparum), can progress rapidly and lead to death if left untreated 2.
Certain groups are at a higher risk of severe infection, including infants, children under 5 years of age, pregnant women, those with HIV/AIDS, and travellers to endemic areas 2.
The early diagnosis and prompt treatment of malaria is crucial for preventing complications and reducing mortality rates 2.
Burden of Disease
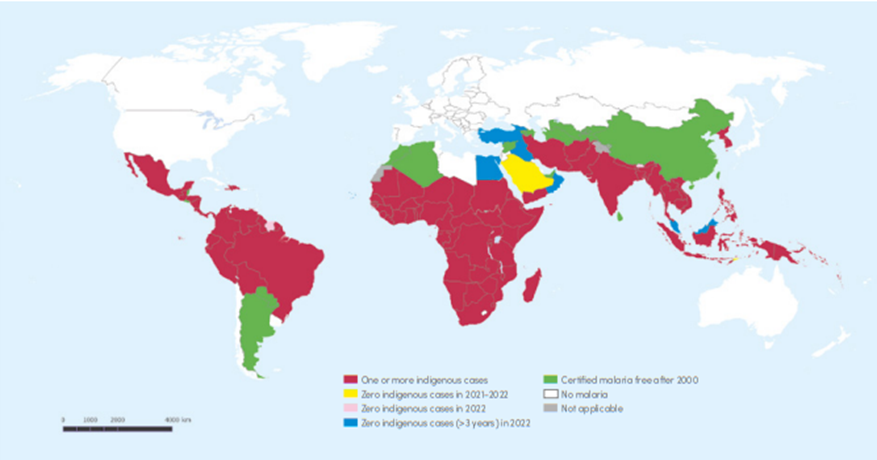
In 2022, there was an estimated 249 million malaria cases and 608,000 malaria-related deaths across 85 endemic countries (see figure 1). 94% (233 million) of global malaria cases and 95% (580,000) of global malaria-related deaths were attributed to the WHO African region 2, 3.
Figure 1: Countries with indigenous cases in 2000 and their status by 2022 3

WHO: World Health Organization
a. Malaysia has a significant number of indigenous malaria cases caused by Plasmodium knowlesi infection.
b. Countries with zero indigenous cases for at least 3 consecutive years are considered to have eliminated malaria. In 2022, Malaysia reported zero indigenous cases caused by human Plasmodium species for the fifth consecutive year and Cabo Verde reported zero indigenous cases for the fourth year. Belize was certified malaria free in 2023, following 4 years of zero malaria cases.
Incidence
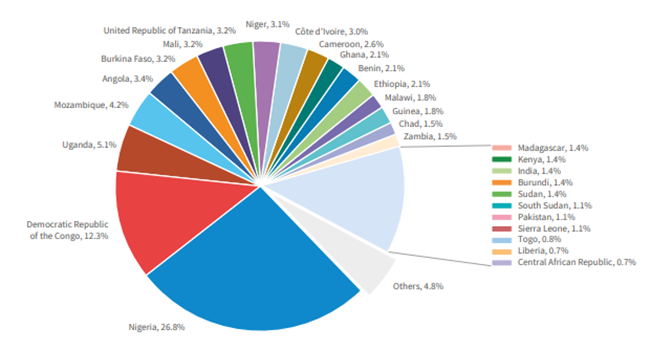
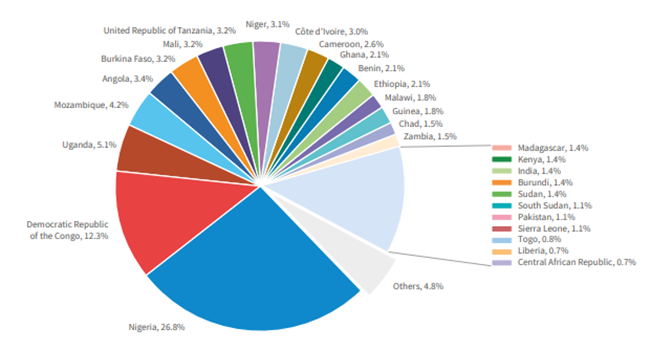
Figure 2 highlights how the burden of malaria is disproportionately concentrated in a few countries, with a significant proportion of cases occurring in just four nations. Of all global malaria cases, Nigeria accounts for 26.8%, Democratic Republic of the Congo (BRC) accounts for 12.3%, Uganda accounts for 4.2% and Mozambique accounts for 4.2%. Together, these four countries collectively contribute almost half of all malaria cases worldwide. This underscores the significant burden of malaria they face and the importance of prevention, diagnosis and treatment to combat the disease effectively in these regions 3.
Figure 2: Global Malaria Cases 3


Between 2021 and 2022, several countries experienced an increase in malaria cases, with notable contributions from Pakistan, Ethiopia, Nigeria, Uganda and Papua New Guinea. Below is a breakdown of the changes in incidence and the factors contributing to the rise in cases 3:
Pakistan 3
- Experienced a significant increase in malaria cases of 2.1 million.
- Incident rose five-fold, from 2.2 to 11.5 cases per 1000 population at risk.
- Contributing factors may include: climate change, healthcare access, and vector control measures.
Ethiopia 3
- An increase of 1.3 million malaria cases.
- Incident rose by 32% from 46.3 to 60.9 cases per 1000 population at risk.
- Contributing factors may include: environmental, healthcare access, and socioeconomic.
Nigeria 3
- An increase of 1.3 million malaria cases, although incidence remained unchanged.
- The rise in cases was primarily attributed to population growth rather than an increase in the incidence rate.
Uganda 3
- An increase of 597,000 malaria cases.
- Incidence rose slightly by 2% from 262.9 to 267.8 cases per 1000 population at risk.
- While the increase in incidence was relatively small compared to other countries, it still represents a significant number of additional cases.
Papua New Guinea 3
- Increase of 423,000 malaria cases.
- Incidence rose by 32%, from 124.3 to 163.7 cases per 1000 population at risk.
- Contributing factors include: environmental changes, insecticide resistance, and challenges in healthcare delivery to remote areas.
Whilst there has been a stabilisation in incidence rates, these increases highlight the ongoing challenges in malaria control and the need for intensified efforts in prevention, diagnosis, and treatment, particularly in regions experiencing rising incidence rates 3.
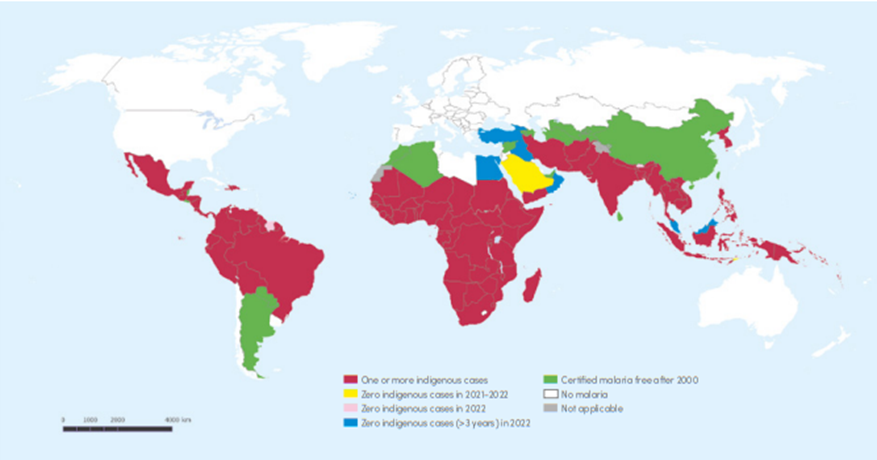
Mortality
Figure 3 below highlights the significant burden of malaria in certain countries with just under a third of global malaria deaths attributed to Nigeria (31.1%). Moreover, four countries account for just over half of global malaria deaths: Nigeria (31.1%), Democratic Republic of the Congo (11.6%), Niger (5.6%) and United Republic of Tanzania (4.4%) 3.
These statistics emphasise the disproportionate burden of malaria-related deaths borne by a small number of countries, with Nigeria once again shouldering the most significant share. The Democratic Republic of the Congo, Niger, and the United Republic of Tanzania also face substantial challenges in combating malaria-related mortality. Furthermore, Nigeria’s alarming percentage of global malaria deaths among children under 5 (38.5%) underscores the critical need for targeted interventions to protect this vulnerable demographic 3.
Figure 3: Global Malaria Deaths 3


Social & Economic Toll
The economic burden of malaria is substantial, affecting both individuals and governments in various ways 4:
Costs to individuals and families 4:
- Purchase of treatment: Individuals often incur expenses in buying drugs for treating malaria, either over-the-counter or prescribed.
- Healthcare expenses: This includes costs associated with seeking medical care at dispensaries or clinics, including consultation fees, diagnostic tests, and hospitalisation if necessary.
- Travel costs: Expenses related to transportation to healthcare facilities for treatment.
- Lost days of work: Malaria can lead to absenteeism from work, resulting in lose income for individuals and their families.
- Education disruption: Absence from school due to illness affects educational attainment and imposes additional costs on families.
- Preventive measures: Costs associated with purchasing preventive measures such as insecticide-treated bed nets or mosquito repellents.
- Funeral expenses: In cases of malaria-related deaths, families may incur expenses for burial arrangements.
Costs to governments 4:
- Healthcare infrastructure: Governments bear the costs of maintaining, supplying, and staffing healthcare facilities for malaria treatment and prevention.
- Procurement of drugs and supplies: Expenses related to purchasing anti-malarial drugs, diagnostic kits, and other medical supplies.
- Public health interventions: Costs associated with implementing public health interventions, such as insecticide spraying, distribution of bed nets, and malaria awareness campaigns.
- Lost productivity: Malaria-related absenteeism leads to lost productivity, affecting economic output and government revenue.
- Impact on economic growth: Malaria’s burden on the workforce and productivity hampers economic growth and development, leading to significant long-term costs.
Over economic impact 4:
- Direct costs associated with illness, treatment, and premature death amount to at least $12 billion USD per year.
- However, the indirect costs, including lost economic growth, are likely to be significantly higher, impacting the overall development of malaria-endemic countries.
Addressing malaria comprehensively not only improves public health outcomes but also contributes to the economic development by reducing healthcare expenses, increasing productivity, and fostering economic growth 4.
Elimination of Malaria
The vision outlines by the World Health Organization (WHO) and the global malaria community is ambitious yet essential for public health. Achieving a world free of malaria required concerted efforts from governments, health organisations, communities, and individuals worldwide 5.
It is recognised that different countries are at various stages in their efforts to eliminate malaria. Progress depends on several factors, including the strength of the national health system, investment in elimination strategies, and socio-economic factors. Additionally, biological determinants such as the mosquito vector’s behaviour and resistance to anti-malarial drugs, as well as environmental factors, play significant roles 5.
As of January 2024, WHO has certified 43 countries and 1 territory as malaria-free. This certification represents significant progress in the global fight against malaria. However, it also underscored the ongoing challenges and the need for continued vigilance and investment to prevent the re-establishment of transmission in these areas 5.
To achieve the vision of a malaria-free world, it is crucial for countries to maintain and strengthen their malaria control and elimination efforts, including surveillance, vector control, access to treatment, and community engagement. Collaboration among nations, international organisations, researchers, and other stakeholders is vital for sharing knowledge, resources, and best practices to accelerate progress towards malaria elimination globally 5.
Importance of Diagnostics
WHO’s recommendation for prompt malaria diagnosis through microscopy or rapid diagnostic tests (RDTs) is crucial for effective disease management and surveillance. This approach allows healthcare providers to distinguish between malarial and non-malarial fevers swiftly, ensuring appropriate treatment and reducing unnecessary use of antimalarial drugs 6.
Parasite-based diagnostic testing not only improves patient care but also contributes to reducing illness and death associated with malaria. By accurately identifying cases, it helps prevent the emergence and spread of drug resistance. This strategy aligns with WHO’s goal of ensuring quality-assured diagnosis, which is essential for effective malaria control and elimination efforts 6.
The increased proportion of patients receiving malaria diagnostic tests since WHO’s recommendation in 2010 reflects progress in implementing this strategy. However, continued efforts are needed to ensure universal access to quality-assured diagnostic testing, especially in areas with limited healthcare infrastructure 6.
By adhering to WHO’s guidelines for malaria diagnosis and treatment, healthcare providers can improve patient outcomes, strengthen surveillance systems, and contribute to global efforts to combat malaria effectively 6.
How Fortress Can Help
Fortress offer ELISAs and rapid tests for the diagnosis of malaria.
Quote our promotional code ‘MALARIA24’ for a discount on Malaria products.
References
- World Health Organization (WHO). Malaria. https://www.who.int/data/gho/data/themes/malaria (accessed 22 March 2024).
- World Health Organization (WHO). Malaria. https://www.who.int/news-room/fact-sheets/detail/malaria (accessed 22 March 2024).
- World Health Organization (WHO). World Malaria Report 2023. https://iris.who.int/bitstream/handle/10665/374472/9789240086173-eng.pdf?sequence=1 (accessed 22 March 2024).
- Centers for Disease Control and Prevention. Malaria’s Impact Worldwide. https://www.cdc.gov/malaria/malaria_worldwide/impact.html (accessed 22 March 2024).
- World Health Organization (WHO). Global Malaria Programme - Elimination. https://www.who.int/teams/global-malaria-programme/elimination (accessed 8 April 2024).
- World Health Organization (WHO). Global Malaria Programme – Diagnostic Testing. https://www.who.int/teams/global-malaria-programme/case-management/diagnosis (accessed 8 April 2024).